PS4 - 03: RESIDENT AUTONOMY IN THE OPERATING ROOM: DOES GENDER MATTER?
Heather E Hoops, MD, Aaron Heston, BS, Elizabeth Dewey, MS, Donn Spight, MD, Karen J Brasel, MD, MPH, Laszlo N Kiraly, MD; Oregon Health & Sciences University
Introduction: Previous studies have identified gender-based differences in resident autonomy in the operating room. The objective of this study was to examine the association between resident and attending gender on intraoperative autonomy during laparoscopic cases.
Methods: This study retrospectively reviewed resident performance and level of guidance during laparoscopic procedures as reported on procedure feedback forms as well as performance on Fundamentals of Laparoscopic Surgery (FLS) tasks from one institution over a 3-year study period (2013-2016). Data collected included resident gender, attending gender, resident post-graduate year (PGY), case characteristics, level of guidance, and resident intraoperative performance in five domains: operative technique, operative knowledge, medical knowledge, communication, and professionalism. Time to complete each of the five FLS tasks during yearly skills labs was also collected. Univariate and multivariate analyses were performed testing for an association between resident and attending gender with level of intraoperative guidance. Multivariate regression analysis controlled for PGY level, case characteristics, resident intraoperative performance, and FLS task performance. Significance was set at p<0.05.
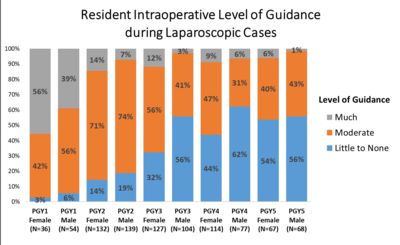
Results: Data were collected from 918 laparoscopic procedures, including intraoperative performance data for 73 PGY1-PGY5 residents (51% female, 49% male), who were evaluated by 94 different attending surgeons (26% female, 74% male). Female resident gender was associated with more guidance needed in the operating room than PGY-matched male residents in both the univariate (p=0.004; see figure) and multivariate analysis (p=0.044). There was no difference between performance of female and male residents on any of the five FLS tasks. Other significant factors affecting level of intraoperative guidance included PGY level (p<0.001), attending ratings of resident operative technique (p=0.001) and operative knowledge (p<0.001) as well as case difficulty (p<0.001). Attending gender was not significantly associated with resident level of guidance.
Conclusions: Gender bias may adversely affect female resident autonomy and attending perception of autonomy in the operating room. This study demonstrated gender-based differences in intraoperative guidance that were present despite controlling for technical performance both intraoperatively and during simulated laparoscopic FLS tasks. Further work is needed to determine factors that contribute to gender-based differences in intraoperative autonomy.