PS3-04: THE INFLUENCE OF ESTABLISHING LEARNING GOALS IN THE OPERATING ROOM
Hailey M Shepherd, BS1, Tawni M Johnston1, Ashley R Allen1, Brigitte K Smith, MD2, Amalia L Cochran, MD3; 1The University of Utah School of Medicine, 2The University of Utah, 3The Ohio State University
Background: Prior studies have addressed various benefits of goal-oriented learning; however, information is lacking on the quality of the learning experience of residents and medical students in the operating room (OR) following the establishment of a learning goal (LG). This study examines the use and impact of trainee-established LGs for resident and medical student training.
Methods: Following IRB approval and a consent prosess, general surgery cases were selected from May 2016 to April 2018 based on resident and medical student involvement. Anonymous surveys were distributed using Research Electronic Data Capture (REDCap) software following case completion to identify current year in training, whether a LG was established prior to the case, if the LG was met, and overall learning experience. Satisfactory learning experience was defined as a 4/5 or 5/5 response on Likert scale with descriptive statistics calculated to characterize differences in learning experiences among participants.
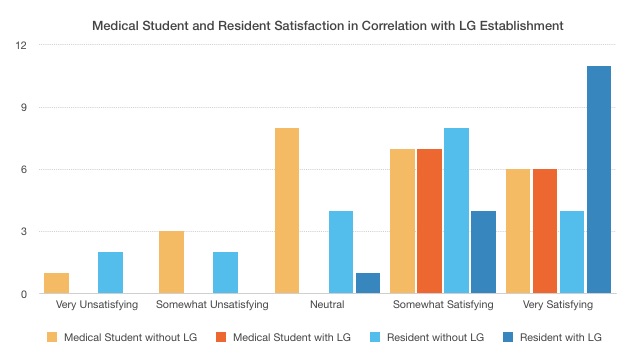
Results: Participants in 65 operative cases were selected for the study, which included 30 attending surgeon responses (49% response rate, n=12), 36 resident responses (55% response rate, n=21), and 54 medical student responses (69% response rate, n=24). Faculty surgeons were most likely to establish a LG for the trainee prior to the case (67%), followed by residents (44%) and students (32%). Medical students reported a satisfactory learning experience in 100% of cases if a LG was established (n=12) and 52% cases if no LG was established (n=25) [Figure 1]. Residents also reported higher learning satisfaction if a LG was established (81% n=13; vs 60% n=12). Faculty surgeons’ perceptions of student and resident satisfaction were lower than satisfaction reported by trainees.
Conclusion: This study demonstrates that early establishment of LGs for medical students and residents is associated with higher rates of satisfaction with overall learning experiences during surgical cases. Medical students were least likely to identify a LG and showed great satisfaction when LGs were identified, and therefore may benefit most from implementing this practice.
Figure 1