PS9-08: PROCEDURAL SKILL COMPETENCE IN GRADUATING MEDICAL STUDENTS: EVOLVING EXPERIENCE AND DESIRES
Monica M Grova, MD, Michael O Meyers, MD; University Of North Carolina At Chapel Hill
Introduction: The AAMC published the Core Entrustable Professional Activities (EPA) guide in 2014, which scaled back recommendations for procedural competence in students. We examined whether student experience or opinion had changed before and after these recommendations.
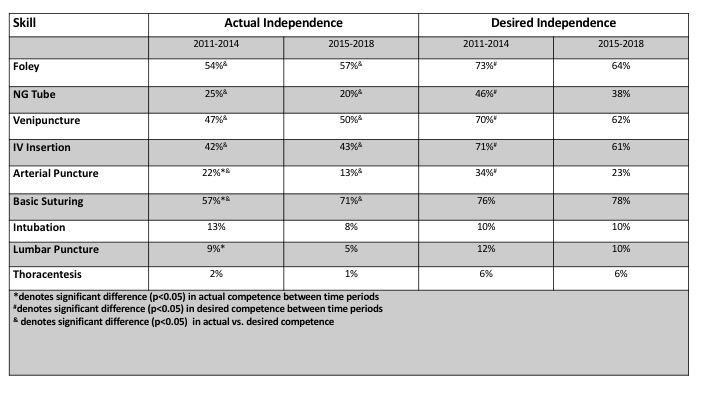
Methods: Under IRB approval, graduating students at a single medical school were queried over an eight-year period via online survey to assess experience as well as actual and desired competence for nine procedural skills (Table). Data were collected on a 4-point scale (4=independently performs to 1=unable to perform) and analyzed by Chi-square and Student’s t-test.
Results: 844 students responded (n=500 2011-2014/n=344 2015-2018). 51% women (55% v. 44% for the two periods;p=0.02). 51% and 54% respectively were pursuing procedural specialties in the two time periods (p=0.36). Personal competence assessed as independent ranged from 62% (basic suturing) to 2% (thoracentesis) and changed over time for arterial puncture (22% vs. 13%; p=0.001), lumbar puncture (9% vs. 5%; p=0.028) and basic suturing (57% vs. 71%; p=0.0001). (Table) A gap in proportion of students desiring to be independent vs. actual level of independence existed for all skills except intubation, lumbar puncture and thoracentesis (p<0.05 for all). (Table) This was no different between the two time periods. However, the proportion of students desiring independence for Foley placement, NG tube placement, venipuncture, IV insertion and arterial puncture decreased between the time periods (p<0.05) (Table)
Conclusions: A majority of students still desire independence in many basic and intermediate procedures. However, there have been small changes in student opinion for many procedures and corresponding decreases in actual independence over time for several procedures.