Plenary1-05: USE OF ERROR MANAGEMENT THEORY TO QUANTIFY AND CHARACTERIZE RESIDENTSâ ERROR RECOVERY STRATEGIES
Carla M Pugh, MD, PhD1, Katherine L Forsyth, PhD2, Elaine R Cohen, MEd3, Anne-Lise D D'Angelo, MD4, Jacob A Greenberg, MD, EdM4, Caprice C Greenberg, MD, MPH4, Douglas A Wiegmann, PhD4; 1Stanford University, 2Mayo Clinic, 3Northwestern University, 4University of Wisconsin - Madison
Background: Traditional checklist metrics for surgical performance can miss key intraoperative decisions that impact procedural outcomes. Error-based assessments may help identify important metrics for evaluating operative performance and resident readiness for independent practice.
Methods: This study utilized human factors error analysis and error management theory to investigate a previously collected video database of resident performance during a simulated laparoscopic ventral hernia (LVH) repair. Senior (PGY 4-5) general surgery residents (N=20) were video recorded while they performed the hernia repair on a table-top simulator using standard laparoscopic tools and mesh. Errors were deconstructed and coded using a structured observation tool and video analysis software. Error detection events and error recovery events were for each operative step of the ventral hernia repair.
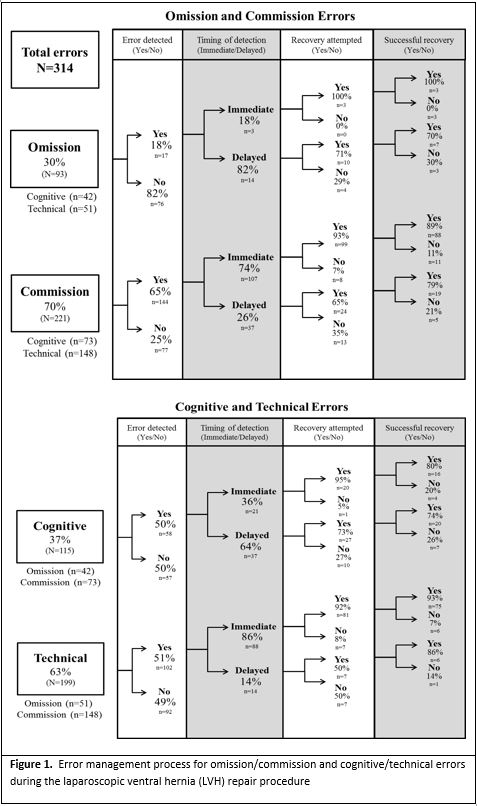
Results: Residents made a total of 314 errors (M=15.7, SD=4.96), Figure 1. There were more technical errors (63%) than cognitive errors (37%) and more commission errors (69%) than omission errors (30%). Almost half (47%) of all errors went completely undetected by the residents for the entire LVH repair. Of the errors that residents attempted to recover (n = 136), 86.0% were successfully recovered. Technical errors were four times more likely to be successfully recovered than cognitive errors (p=.020).
Conclusions: Our results revealed specific details regarding residents’ error management strategies and provides validity evidence for the use of human factors error frameworks in surgical performance assessments. Practice in simulation-based learning environments may improve resident decision-making and error management opportunities by providing a structured experience where errors are explicitly characterized and used for training and feedback. Error management training may play a major role in equipping residents and junior faculty with the skills required for independent, high-quality operative performance.