Plenary2-04: MEANINGFUL AUTONOMY IN GENERAL SURGERY TRAINING: EXPLORING FOR GENDER BIAS
Samantha Lane, MHS, Sarah Hayek, MD, Katelyn Young, BS, James Dove, BA, Nicole Sharp, MD, Mohsen Shabahang, MD, PhD, Halle Ellison, MD; Geisinger
Introduction: Progressive intra-operative autonomy is an educational imperative in a residency program. Recent studies demonstrated female cardiothoracic surgical residents were less likely to receive meaningful autonomy (MA) from faculty compared to male residents. The purpose of this study is to analyze gender differences in the amount of operative MA given to general surgery trainees.
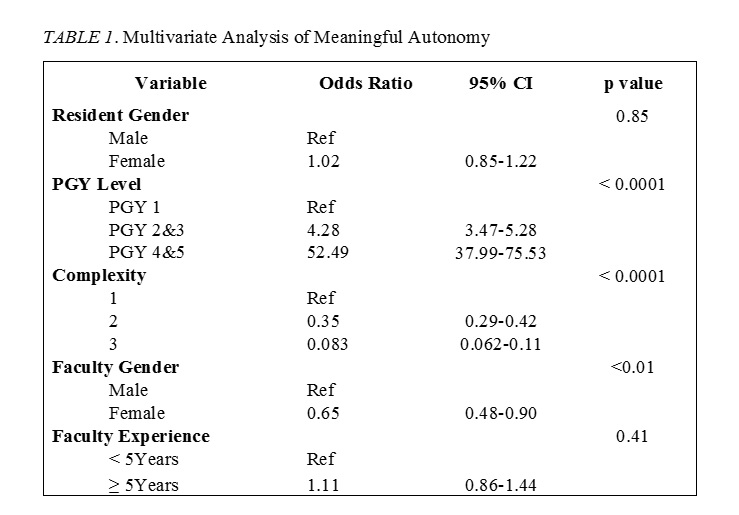
Methods: This is a retrospective study of general surgery residents (17 female, 18 male) at an academic tertiary care facility. Attending surgeons (15 female, 37 male) completed post-operative autonomy evaluations based on the Zwisch model (4-point scale, ≥3 indicating MA). Multivariate analysis was completed using post-graduate year (PGY) level, case complexity (rated 1-3 for increasing complexity), faculty experience, and resident/attending gender.
Results: A total of 3,574 evaluations were analyzed (1,380 female, 2,194 male residents). Female faculty completed 294 evaluations and male faculty completed 3,280 evaluations.
Upon univariate analysis, female residents had a higher incidence of MA with both male (p < 0.0001) and female faculty (p= 0.002). Female residents had a higher incidence of MA in all 3 case complexity levels (p <0.0001) and higher incidence with experienced faculty (p <0.0001).
Multivariate analysis revealed several factors associated with MA (Table 1). The likelihood of receiving MA decreased for case complexities ≥2 when completed with female faculty and increased for residents who were PGY ≥2. Resident gender and faculty experience level had no significant effect on MA.
Conclusion: In contrast to previously published literature, we found that resident gender does not influence MA. The amount of MA was influenced by case complexity and PGY level.