Poster1-01: ERGONOMICS DRIVEN TRAINING: CAN WEARABLE SENSORS GUIDE ROBOTIC SKILLS TRAINING?
Jackie S Cha, MSE1, Jay Sulek, MD2, Chandru P Sundaram, PhD2, Xiayu Cai1, Juan Wachs, PhD1, Denny Yu, PhD1; 1Purdue University, 2Indiana University School of Medicine
Introduction: The demand for robotic surgery is rapidly increasing, but it is a difficult technique to master. Current robotic surgical education programs include simulated skills training with post-exercise performance feedback on task performance metrics (e.g., motion economy, completion time); however, there are no scores on ergonomics. We hypothesize that individual ergonomics, measured using objective sensors, can impact performance and provide novel feedback on contributors to poor performance and improve training.
Methods: Data collection was completed in simulation and operating room (OR) environments in 1 large academic hospital. Electromyography (EMG) sensors obtained upper body muscle activity: left and right neck, shoulder, bicep, and forearm. Signals were normalized across subjects using percent maximum voluntary contraction (MVC). Twelve simulation exercises were completed on the da Vinci Simulator and performance scores were recorded. Partial nephrectomy procedures were also collected. Pearson correlation and multiple regression analysis were used to determine the effect of muscle activity on simulation skills performance. Muscle activity during simulated suturing exercises and during kidney reconstruction was compared using t-tests to test whether simulation ergonomics is representative of OR ergonomics.
Results: Eight trainees participated between 4 to 5 simulation sessions for a total of 208 exercises. Six cases in the OR performed by 2 surgeons were also collected. Muscle activity for neck and left bicep (Figure 1) were significantly negatively correlated with performance score (r2=0.02-0.04, p<0.05). Multiple regression model of EMG metrics yielded r2=0.25. Significant differences (p<0.05) of the static muscle load of both arms were found between the two environments; however, differences were not significant for high force exertions.
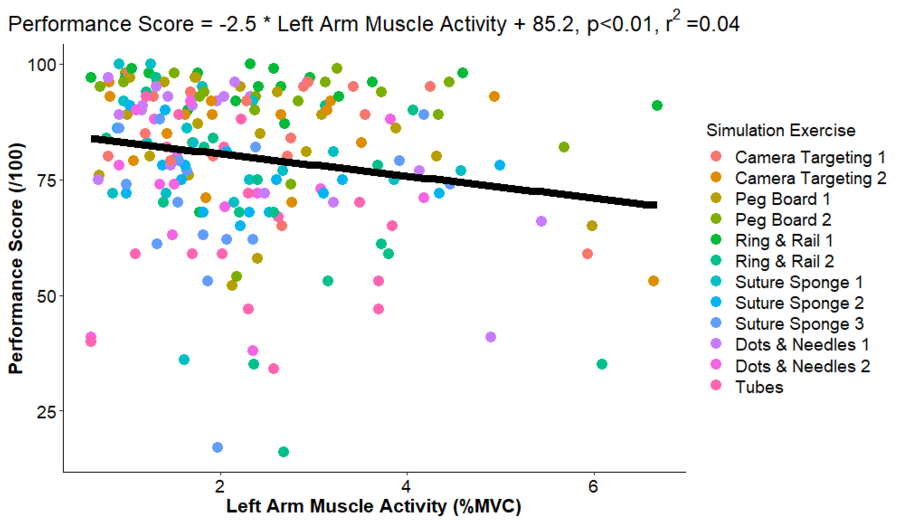
Conclusions: Muscle activity does impact trainee performance, with higher force negatively correlated with performance. Non-dominant arm activity was especially important during simulated skills performance and suggests additional training emphasis is needed on this arm to be more ambidextrous and improve performance. Comparison of the suturing tasks in simulation and OR show that though static load is different, the suturing exercises simulate the dynamic task muscle activity requirements of the surgical procedures. Ergonomics can be a metric of performance of trainees and can be leveraged to develop effective training exercises and programs.
