Poster1-05: EVALUATION OF THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA (AAST) SEVERITY GRADING SYSTEM FOR COMMON EMERGENCY GENERAL SURGERY (EGS) CONDITIONS - A PILOT STUDY OF STANDARDIZED DATA COLLECTION PROCESSES
Kovi E Bessoff, MD, PhD1, Sylvia Bereknyei Merrell, DrPH, MS2, Aussama K Nassar, MD, MSc, FRCSC, FACS3, David A Spain, MD, FACS3, Lisa M Knowlton, MD, MPH3; 1Stanford University School of Medicine, Department of Surgery, Division of General Surgery, 2Stanford University School of Medicine, Department of Surgery, Stanford-Policy Improvement Research and Education Center (S-SPIRE), 3Stanford University School of Medicine, Department of Surgery, Section of Trauma & Critical Care
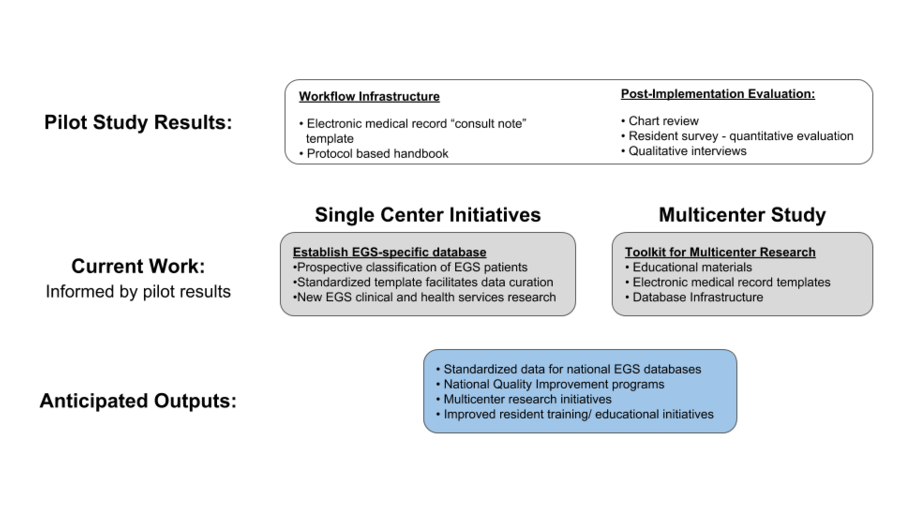
Background: Emergency general surgery (EGS) encompasses an anatomically diverse set of diseases, the management and outcomes of which vary across institutions. Lack of a standard severity classification system limits the organization of a database to study operative and non-operative outcomes. This led the AAST to develop a uniform anatomic severity grading system for common EGS conditions. Its utility, however, has not been validated prospectively. We hypothesized that integration of the EGS classification system into our clinical workflow could: (1) improve data collection, and (2) provide educational value by increasing residents’ confidence toward patient management, and improving resident-attending communication (Figure).
Methods: We developed a consult note template and standard operating guidelines for the management of common EGS conditions. ?Residents prospectively assigned an EGS classification at the time of patient evaluation, initiated protocolized treatment, and documented findings using the standardized EGS template. ?At one-year post-implementation, residents were electronically surveyed to assess satisfaction and feasibility. Follow-up interviews of residents and surgeons were conducted to clarify survey responses.
Results: At one year, 438 patients (estimated 30% of all EGS consults) had been assigned a standardized EGS classification in their consult note. This cohort included patients who were managed operatively and non-operatively. 15 residents (70%) completed the survey and 53% (n=8) of respondents felt that integration of the EGS classification system and care protocols into the clinical workflow was useful. However, only 27% (n=4) of respondents reported significant benefit regarding resident-attending communication, suggesting the need to establish more robust frameworks and protocols to facilitate clinical communication. Follow-up interviews with residents and surgeons identified barriers to implementation of the new workflow and areas for improvement to promote widespread adoption.
Conclusion: Our study demonstrated the feasibility of integrating an EGS classification system into clinical documentation. Such a system has the potential to facilitate clinical workflow, and support quality improvement and prospective research. The successful implementation of such a toolkit may then be scaled across hospitals, thereby promoting future multicenter collaboration and facilitating the establishment of a national EGS database (Figure).