Poster4-08: THE INTEGRATED THORACIC RESIDENCIES ARE REDUCING TRADITIONAL CARDIOTHORACIC âFELLOWSHIPâ TRAINING OPPORTUNITIES AT TOP PROGRAMS
Lynze R Franko1, Catherine M Gilbert1, Reilly Hobbs, MD2, Rishindra M Reddy, MD2; 1University of Michigan Medical School, 2University of Michigan Dept of Thoracic Surgery
Purpose: Cardiothoracic (CT) training programs have broadened to include integrated 6-year programs (IPs) since 2007. Students are concerned about the reduction in top traditional program (TP) “fellowship” spots after general surgery (GS) training and feeling pushed towards applying to IPs. We sought to understand the impact of IPs on the number and quality of TP positions.
Methods: Publicly available data from Accreditation Council for Graduate Medical Education and National Resident Matching Program was used to determine the number of positions in TPs and IPs from 2007 – 2018 and to evaluate medical students applying to GS and IP. CT programs were ranked into 3 tiers (1=top) utilizing Doximity’s GS rankings and a focus group of CT surgeons.
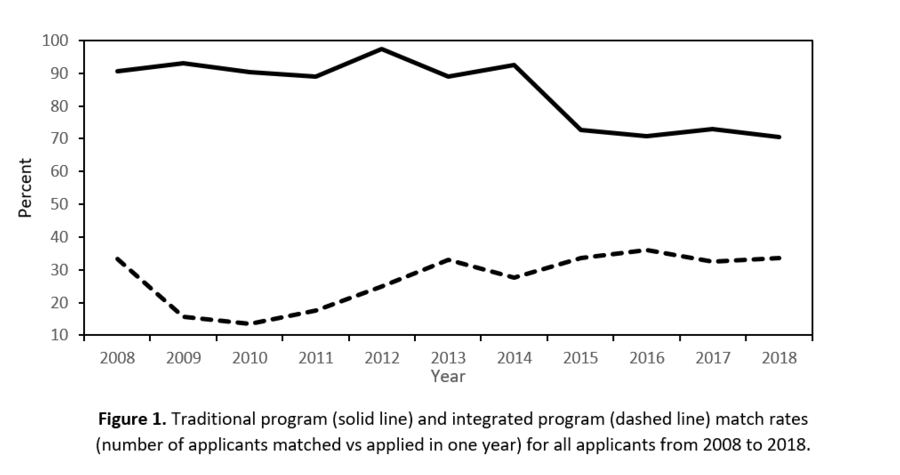
Results: CT traditional programs have decreased from 81 in 2007 to 72 in 2017. The number of filled positions over all years (PGY1-6) for TPs decreased from 246 to 224. There are currently 97 TP graduates (2017) compared to 118 (2007), a 17.8% reduction. Since 2007 26 IPs have developed. In 2017 IPs have 36 PGY1 filled positions, 183 filled over all positions (PGY1-6), and 21 graduates. At tier 1 TPs (n=16) 10 have developed IPs with 16 IP spots/year. The filled positions over all years at tier 1 TPs have decreased from 88 to 68, a 22.7% reduction. Tier 2 and tier 3 TP filled positions have been stable at 76 and 80 (2007) to 79 and 79 (2017), respectively. Since 2007, the number of TP applicants increased from 96 to 126. The corresponding match rate for TPs has decreased from 90.6% to 70.6% (Figure). The number of IP applicants have gone from 9 to 107 with a current match rate of only 43%.
Conclusions: Despite the perception that CT training opportunities are unchanged for GS residents by the introduction of the IPs, the number of training positions at top tier TPs has been reduced. Some students may feel compelled to apply to IPs despite an interest in GS training first. Closer monitoring of how changing training opportunities affects medical student career selection is needed.