Poster5-02: GENERAL SURGERY RESIDENT EXPERIENCE WITH ANORECTAL SURGERY
Asya Ofshteyn, Morgan Terry, Katherine Bingmer, Sharon L Stein, Emily Steinhagen; Case Western Reserve University/University Hospitals Cleveland Medical Center
Background: Previous studies have suggested that general surgery residents graduate with suboptimal anorectal experience. As more anorectal surgery is performed in ambulatory settings, there is concern that fewer anorectal procedures are performed while training residents. The increase in number of postgraduate colon and rectal residents also potentially decreases general surgery resident exposure. However, competence in anorectal procedures is an important part of general surgery training.
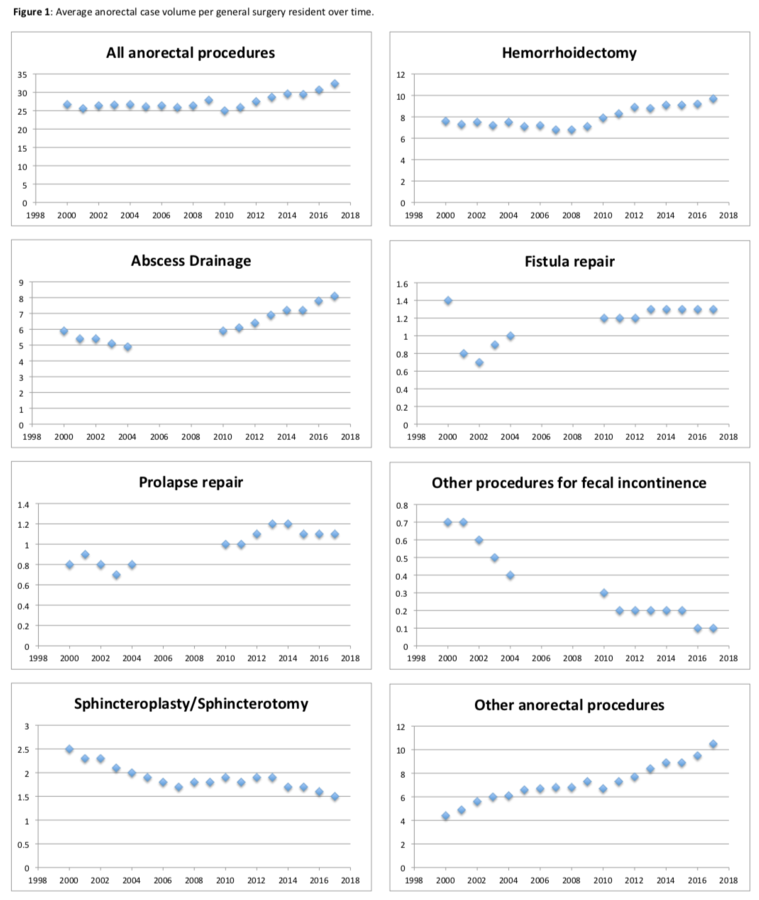
Methods: ACGME general surgery resident case logs from 1999 to 2017 were reviewed. The mean number of anorectal procedures including hemorrhoidectomy, fistulotomy, abscess drainage, sphincterotomy/sphincteroplasty, prolapse procedures, fecal incontinence procedures, other anorectal procedures, and total anorectal procedures combined were evaluated. Between 2005 and 2010, there was a change categories that resulted in gaps in fistula, abscess drainage, prolapse and fecal incontinence procedure datasets.
Results: Between 1999 and 2017, the mean number of all anorectal procedures performed by each general surgery resident has increased from 25.9 to 32.4 – a 25% increase (Figure 1). There is a positive trend in the mean number of all anorectal procedures performed starting in 2009. A similar trend is seen in hemorrhoidectomy (7.6 to 9.7, 28%), abscess drainage (5.9 to 8.1, 37%), and other procedures (4.4 to 10.5, 139%). Prolapse procedures (0.8 to 1.1, 27%) and fistula repair (0.8 to 1.3, 63% without initial outlier) appear to have increased but the trend is less linear. Sphincterotomy/sphincteroplasty (2.5 to 1.5, -44%) and fecal incontinence procedures (0.7 to 0.1, -86%) appear to be decreasing.
Conclusions: General surgery residents have gained more experience in some anorectal procedures over time. This occurred despite the rise in colon and rectal residents and increase in procedures performed in ambulatory settings. The required number of procedures to establish competence is not well defined and should be formally evaluated.