Plenary - 02: MIND THE GAP: A PILOT STUDY - A DIVERGENCE BETWEEN FULL ENTRUSTABILITY AND PERCEIVED AUTONOMY FOR SURGICAL RESIDENTS IN THE OR
Gurjit Sandhu, PhD1, Julie A Thompson-Burdine, BA1, Niki Matsuko, BS1, Danielle C Sutzko, MD, MS1, Vahagn C Nikolian, MD1, Anna Boniakowski, MD1, Patrick E Georgoff, MD1, Kaustubh A Prabhu, BA1, Rebecca M Minter, MD2; 1University of Michigan, 2UT Southwestern
Background/Purpose: Problematically, 25% of surgery residents believe the current curriculum does not prepare them to practice as independent surgeons. Faculty entrustment decisions affect how resident entrustability is exhibited, which in turn determines the degree to which trainees gain intraoperative responsibility and surgical autonomy. While garnering increasing investigation, the transition from entrustability to autonomy is not well understood. This pilot study explores the relationship between observed resident entrustability behaviors and self-perceived autonomy among surgical residents.
Methods: At the University of Michigan, September 2015 - June 2017, 226 surgical observations were completed. 56 faculty and 73 residents were observed across four surgical specialties: general, plastic, thoracic, and vascular. Entrustment behaviors were rated using OpTrust, a validated objective entrustment measurement tool. Purposeful sampling generated variation in operation type, case complexity, faculty-resident pairings, and resident training level. At the completion of each case, residents were asked to complete a Zwisch self-assessment to measure surgical autonomy.
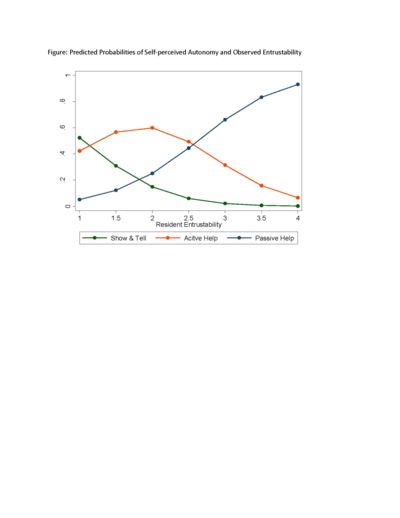
Results: Full entrustability was observed in the OR; however, residents in our study did not report full autonomy in self-assessments. Spearman’s rank correlation coefficient identified resident entrustability was positively correlated with perceived resident autonomy (ρ=0.66, p < .05). Ordinal logistic regression was used to assess the relationship between resident entrustability and autonomy. The relationship persisted while controlling for PGY level, gender, and case complexity (or=8.42, se=4.54, p < 0.000). The predicted probability of perceiving “show and tell” decreased as entrustability increased. The predicted probability of perceiving “active help” first increased as entrustability increased, but then decreased. The predicted probability of perceiving “passive help” increased as entrustability increased. No “supervision only” data was reported. (Figure)
Conclusions: Resident entrustability is positively associated with perceived autonomy, yet full entrustability is not translating to the perception of full autonomy for residents. A more detailed mapping of how entrustment behaviors and perceived autonomy align will enable surgical educators to advance clinical training. OpTrust is able to detect areas of opportunity for increasing resident entrustability. If areas for improvement can be identified, there is potential to increase entrustability behaviors that result in higher resident self-confidence and a stronger belief in one’s ability to perform autonomously.