Plenary1-04: RESIDENT TRAINING EXPERIENCE WITH ROBOTIC ASSISTED TRANSABDOMINAL PREPERITONEAL INGUINAL HERNIA REPAIR
Peter Ebeling, MD, Katherine Beale, MD, MPH, Kent Van Sickle, MD, Mohammed Al-Fayyadh, MD, Ross Willis, PhD, Juan Marcano, MD, Jason Kempenich, MD; University of Texas Health Science Center-San Antonio
Introduction: General surgery is the fastest growing field in the adoption of robotic assisted laparoscopic surgery, presenting challenges to measuring trainees’ progress toward achieving proficiency. Here, we present the results of one institution’s experience in training surgical residents in robotic assisted transabdominal preperitoneal repairs.
Methods: From March 2017 through August 2018, data were prospectively collected on patients of two attending general surgeons undergoing unilateral or bilateral robotic assisted laparoscopic inguinal hernia repair with surgical trainees. In cases of bilateral inguinal hernias, the attending surgeon did one side, and the resident surgeon did the contralateral side either to completion or until attending takeover. Data points included patient age, gender, complications, hernia difficulty, resident technical competency as measured by the Global Evaluative Assessment of Robotic Skills (GEARS), Zwisch scores, operative time, and the number of robotic console cases self-reported by residents as primary surgeon.
Results: Twenty-six residents participated in the study. Residents performed 64 operations; attending surgeons performed 36. Mean operative times for residents were significantly longer than attendings (53.9 vs 30.5 minutes, p<.001). Operation difficulty did not differ between residents and attending surgeons in the case of bilateral hernias. Residents who completed 10 or fewer total robotic console cases achieved significantly lower mean GEARS and Zwisch scores than those who had completed 11 or more (p<.001). Attending surgeons completed parts of the case significantly more frequently when residents recorded lower GEARS and Zwisch scores (p<.001) or when residents logged fewer cases (p<.05). Case difficulty did not predict attending take over.
Table 1
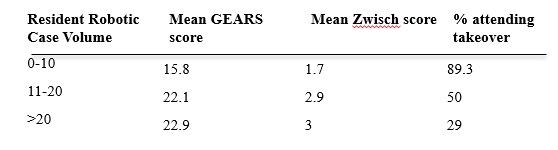
Discussion: As robotic assisted surgery becomes more common, surgery residency programs face the challenge of educating trainees in open, laparoscopic and robotic assisted techniques. Here, we have shown that experienced staff surgeons have shorter operative times compared to surgical trainees, as is expected. Proficiency and autonomy scores increase significantly as surgical trainees gain experience operating with the robot. Accordingly, attending surgeons grant more autonomy to residents with higher proficiency scores