C1 - 12: MITIGATION OF LEARNER ANXIETY AFTER SIMULATION DEATH: IMPORTANCE OF SYSTEMATIC DEBRIEFING
Joseph C L'Huillier1, Sasha M Jascor1, Sarah A Sullivan, PhD2, Ann P O'Rourke, MD, MPH2, Amy E Liepert, MD2; 1University of Wisconsin School of Medicine and Public Health, 2University of Wisconsin Department of Surgery
Introduction: Simulator death during simulation-based medical education remains controversial. Exposure increases learner anxiety and their risk for psychological distress during simulation, which may negatively impact learning. Successful debriefing after simulation may reduce participant anxiety following simulator death while maximizing learning outcomes.
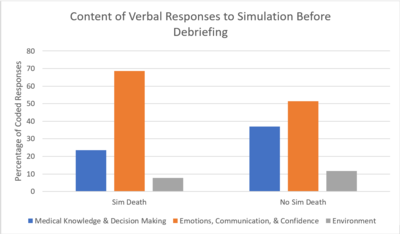
Methods: Nineteen fourth-year medical students individually participated in a clinical decision-making simulation. Facilitators then led an individual debriefing session using the Gather-Analyze-Synthesize model. Each learner completed the State portion of the State-Trait Anxiety Inventory to assess anxiety before simulation and after debriefing. The Cato Confidence Scale was completed by learners after debriefing. Learners’ verbal responses to the experience immediately following the simulation but before debriefing were transcribed, analyzed for sentiment, and coded as pertaining to (1) medical knowledge and decision making, (2) emotion, communication, and confidence, and/or (3) environment. The reduction in State anxiety (pre – post), Cato confidence, and sentiment and content of learners’ responses were compared between those who did and did not experience simulator death.
Results: Six learners experienced simulator death (SimD) and thirteen did not experience simulator death (NoD). There was no difference between the average reduction in State anxiety (pre – post) between SimD (M=1.67, SD=2.58) and NoD (M=2.17, SD=3.07; p=0.723). Confidence was similar between SimD (M=2.82, SD=0.906) and NoD (M=3.10, SD=0.690; p=0.519). Verbal responses to the simulation before debriefing produced 13 responses in SimD and 44 in NoD. For SimD, 7/13 (53.8%) of their responses contained negative sentiment (eg. “Oh my God—I’m going to kill someone. They should not graduate me. I am literally having a panic attack.”) whereas 14/44 (31.8%) of NoD responses contained negative sentiment (eg. “Overall I felt like I had a pretty good grasp on the patient and where she was going”). The coded content of their responses can be seen in Figure 1.
Conclusion: Successful debriefing mitigated the increased anxiety as detected by increased negative sentiment among those who experienced simulator death. Exposure to simulator death shifted the content of learner responses from knowledge based to a more emotional basis. Structured debriefing may allow learners to benefit from experiencing death while reducing their risk of psychological harm.