C2B - 10: A SINGLE CADAVER SIMULATION LABORATORY SIGNIFICANTLY IMPROVES RESIDENT COMFORT WITH INTRAVASCULAR SHUNT PLACEMENT IN TRAUMA
J A Savarese, MD, W C Beck, MD, A Bhavaraju, MD, M K Kimbrough, MD, K W Sexton, MD, M C Elkins, J R Taylor, III, MD; University of Arkansas for Medical Sciences
Background: In civilian trauma, intravascular shunt placement is a low incidence procedure performed in high acuity settings. Through a trauma case discussed at morbidity and mortality conference, a knowledge gap was identified in the technical aspects of shunt placement. We hypothesized that a cadaver based simulation lab would improve resident facility with this procedure.
Methods: General surgery residents (n=11) ranging from PGY-2 to PGY-5 levels were instructed using a cadeveric model on intravascular shunt placement into the femoral, carotid, and subclavian vessels. The course covered indications, contraindications, dissection, shunt selection, operative technique, securing the shunt, ensuring patency, and managing complications. Participants completed a survey prior to and following the course. Using a Likert scale, surveys were graded on scoring scale from 0 (extremely uncomfortable)-4 (extremely comfortable) to judge comfort level regarding indications, landmarks, complications, exposure, dissection, selection, and technique in placing intravascular shunts. Data were analyzed using GraphPad Prism Version 7.01.
Results: The number of intravascular shunts placed by residents in elective settings was 0 for 54% of participants and 100% of participants had never placed an intravascular shunt under emergent or traumatic situations. A two-way ANOVA test was performed demonstrating significance in pre and post resident comfort for indications (p=.001), landmark identification (.0003), complications (p<.0001), exposure (p<.0001), dissection (p<.0001), selection (p<.0001), and technique (p<.0001) in placing intravascular shunts. The greatest improvement between the pre- and post-surveys were in selection (median 0 to 3) and technique (median 0 to 3).
Conclusions: This study identified a need for simulation with placement of vascular shunts during trauma (0% of residents had placed an emergent intravascular shunt) and demonstrated that a single simulation experience could improve resident comfort for the placement of intravascular shunts. Further work should be done to determine if improved comfort translates to improved clinical outcomes.
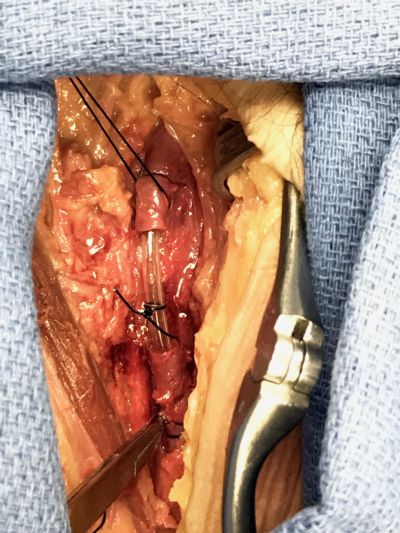
Image 1. Dissection performed during workshop of femoral artery with intravascular shunt in place.
