C3 - 01: GREATER FACULTY-RESIDENT FAMILIARITY IMPROVES INTRAOPERATIVE ENTRUSTMENT
Gurjit Sandhu, PhD1, Julie A Thompson-Burdine, BA1, Vahagn C Nikolian, MD1, Danielle C Sutzko, MD, MS1, Patrick E Georgoff, MD1, Anna Boniakowski, MD1, Kaustubh A Prabhu, BS1, Niki Matusko, BS1, Rebecca M Minter, MD2; 1University of Michigan, 2UT Southwestern Medical Center
Background: Longitudinal contact between faculty and residents has been identified as a factor that facilitates greater faculty entrustment. Entrustment develops slowly over time, but in large programs, faculty experience with a particular resident can be limited. Residents cycle through numerous services with various faculty; the impact of this structure on entrustment has yet to be fully explored. We hypothesize that the degree of entrustment faculty members exhibit toward a given resident is impeded when there is insufficient exposure. The purpose of this study is to assess the relationship between faculty familiarity with residents and faculty entrustment using OpTrust, a validated tool designed to assess progressive entrustment in the operating room (OR).
Materials and Methods: Researchers observed elective surgical cases and rated entrustment behaviors using OpTrust from September 2015 – June 2017 at the University of Michigan. Purposeful sampling was used to generate variation in operation type, case difficulty, faculty-resident pairings, faculty experience, and resident training level. Faculty familiarity with resident and faculty entrustment were each measured on a 1-4 scale where 1=not familiar/low entrustment, 4=extremely familiar/full entrustment. Analysis of variance (ANOVA) and Sidak adjusted multiple comparisons were used to assess the relationship between faculty familiarity and faculty entrustment.
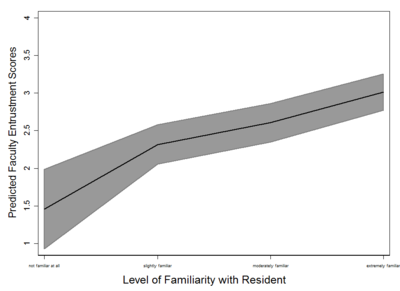
Results: 56 faculty and 73 residents were observed across 225 surgical cases from four surgical specialties: general, plastic, thoracic, and vascular surgery. There was a significant increase in entrustment as familiarity increased: 0.86 for slightly familiar, 1.15 for moderately familiar, and 1.55 for extremely familiar (p=.027, p<.001, p<.001) when compared to not familiar at all (Figure).
Conclusions: This study demonstrates a positive relationship between faculty/resident familiarity and intraoperative entrustment. These findings support greater continuity in faculty/resident relationships. Longitudinal contact allows learners to demonstrate competency and to be granted progressive entrustment by faculty. Greater entrustment allows for safe struggle and greater resident leadership, factors which support effective teaching.
Figure