C3 - 08: MASS CASUALTY PREPAREDNESS EDUCATION AND TRAINING IN GENERAL SURGERY RESIDENCIES
Melissa Linskey Dougherty, MD, Cheyenne C Sonntag, MD, C James Holliman, MD, Eugene Lengerich, VMD, MS, Steven R Allen, MD; Penn State College of Medicine
Background: Mass casualty incidents (MCI) stem from a variety of events, including multiple vehicle accident, mass shooting, structural collapse, natural disaster, or terrorist attack. Although sensational, the incidence of MCI events is relatively low. With limitations on time and resources available for surgical resident education, MCI education and response training may be overlooked or considered low priority. A lack of MCI education and training may negatively affect general surgery resident ability to triage and establish treatment priorities for large volumes of patients.
Objective: To quantify mass casualty education provided in general surgery residency curriculums nationwide. To describe the impact of MCI training on residents’ comfort level with future MCI response.
Methods: A self-administered, anonymous online survey was distributed via online communities and APDS to general surgery residents. Standard descriptive univariate statistics were utilized to find associations between demographics, program characteristics, and mass casualty training. Comfort levels were compared based on participation in drills. P-values less than 0.05 were considered significant.
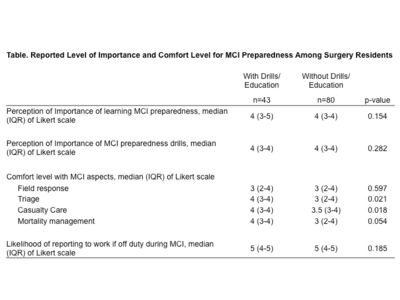
Results: Of the 123 responding residents, 35% reported participation in residency and/or institutional MCI drills. There was no difference in postgraduate level of training, type or region of program, trauma center designation, previous military, emergency responder or international disaster experience among respondents. Residents assigned similar ratings of importance of MCI education and drills, as well as likelihood of reporting to work during MCI. Residents that participate in MCI drills reported higher rates of triage training and involvement in tabletop exercises. Respondents that participate in MCI drills reported higher comfort levels with triage and casualty care (See table).
Conclusions: Only 35% of general surgery residents reported participation in residency or institutional drills for mass casualty preparedness. Despite several recent MCI events such as the Boston bombings and high-profile mass shootings, preparedness training within general surgery programs remains low. Surgery residents desire MCI education and drill participation. Residents who participate in MCI drills report higher comfort with triage and casualty care. More standardized institution of MCI response training during residency can provide increased readiness for these events.