PS3 - 05: COMPARISON OF FACULTY VERSUS STRUCTURED PEER FEEDBACK FOR ACQUISITION OF BASIC AND INTERMEDIATE-LEVEL SURGICAL SKILLS.
Guy Sheahan, MBBS, Richard Reznick, MD, MEd, FRCSC, FACS, Don Klinger, BSc, BEd, PhD, Leslie Flynn, MD, MMus, CCFP, FRCPC, Boris Zevin, MD, PhD, FRCSC; Queen's University
Background: Video feedback and faculty feedback has been shown to result in improved surgical performance; however, consistent access to faculty feedback remains a challenge. We therefore studied the utility of structured peer feedback compared to faculty feedback during acquisition of basic and intermediate level surgical skills.
Methods: A prospective randomized non-inferiority trial was conducted with 1st and 2nd year medical students learning skin lesion excision and closure, and single-layer hand-sewn bowel anastomosis, respectively. Peer feedback participants were trained to use the Objective Structured Assessment of Technical Skills (OSATS) tool to facilitate feedback. An instructional video demonstrating each procedure was shown. Participants performed a minimum of 5 attempts with feedback provided after each attempt. Integrity of the bowel anastomosis and skin closure was assessed. Recorded operative performance was subsequently assessed by two blinded trained raters using the OSATS tool. Non-parametric analysis was used to compare composite scores reflective of overall technical skill.
Results: For each task, 8 participants were randomised to receive faculty feedback and 7 to peer feedback. There were no significant differences between groups at baseline (bowel (p=.622); skin (p=.180)), or on the 5th attempt (bowel (p=.284); skin (p=.589)). Inter-rater reliability for OSATS scores was 0.762 (p<.0001).
|
Bowel Study: |
Bowel Study: |
Skin Study: |
Skin Study: |
|
| OSATS improvement* |
10.3(11.0) p=.017 |
9.5(7.0) p=.043 |
5(5.0) p=.026 |
18.5(23) p=.075 |
| Time improvement* (mins) |
2.5(9.0) p=.309 |
5.7(32) p=.225 |
25.5(15.0) p=.028 |
24.0(39.0) p=.043 |
| Pressure improvement* (cmH20) |
32.5(7.6) p=.012 |
23.0(56) p=.028 |
*Median(IQR), intergroup comparison p>.180
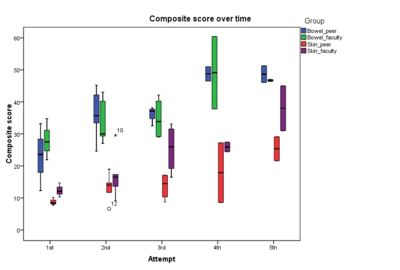
Discussion: Both peer feedback and faculty feedback led to similar and significant improvement in medical student performance in bowel anastomosis and skin lesion excision. Our results suggest peer feedback is equivalent to faculty feedback if specific reference criteria for feedback are taught to the peer group.
