Poster2 - 08: ROBOTIC SURGICAL SKILLS DEVELOPMENT IN GENERAL SURGERY RESIDENTS USING SIMULATION AND 3D-PRINTED ANATOMICAL MODELS
Praveen Sridhar, MD, Virginia R Litle, MD, Kei Suzuki, MD; Boston University Medical Center
Introduction: There has been an increase in the volume of robotically performed surgical procedures; however, resident training in robotic surgery is variable secondary to barriers to intraoperative teaching. Barriers include the lack of a second console, the inability for multiple operators, the need for a bedside assistant, and the acuity of potential complications. We aim to implement a robotic simulation curriculum combining virtual reality simulation and procedure specific simulation using 3D printed anatomical models that mimic operative scenarios. We hypothesize that combined simulation develops basic skills and provides a realistic learning experience despite the barriers to trainee robotic console use.
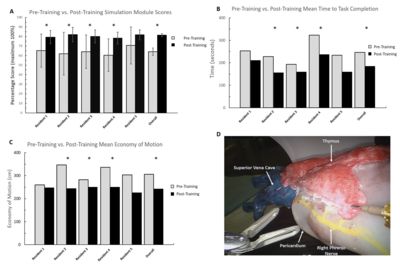
Methods: Our study cohort consists of 30 general surgery residents from our institution. Residents participate in an organized curriculum composed of 16 modules from the robotic skills simulator. Residents repeat modules to achieve a score of 70% based on 20 simulation metrics. These include time to completion (seconds), economy of motion (cm), workspace range (cm), and blood loss (mL), to name a few. Residents perform mock robotic thymectomy on a mediastinal 3D-printed model after completion of simulation training. Residents are then objectively scored based procedure-specific scoring system modeled after a previously validated to score system created to assess technical bronchoscopy skills.
Results: Five residents have completed at least 50% of the simulation curriculum, and one resident has completed a mock robotic thymectomy. Pre-and post-training overall score (Fig 1A. 64.09 vs. 81.47; p<0.005), time (Figure 1B. 246s vs. 185s; p<0.005), and economy of motion (Figure 1C. 306cm vs. 243cm; p<0.05) are displayed. The mean and median number of attempts taken for minimum passing score for all residents across all modules was 2.6 and 2, respectively. Figure 1D displays the mock robotic thymectomy model.
Conclusions: Virtual Reality based simulation is effective in improving basic robotic surgical skill in general surgery residents. Additionally, 3D-printed models can be a valuable tool for procedure-specific training given barriers to intraoperative resident console experience.
